Carbon monoxide: The ‘silent killer’
You can’t smell it, taste it or see it, but it can be deadly. Carbon monoxide – sometimes referred to as the “silent killer” – prevents oxygen from going into the body and can result in death in a short period of time, the Michigan Department of Community Health states. But how does carbon monoxide form, and when are workers at risk?
Carbon monoxide is predominantly produced through incomplete combustion of carbon-containing materials, according to NIOSH. “Incomplete combustion occurs when insufficient oxygen is used in the fuel (hydrocarbon) burning process,” NIOSH states, adding that, consequently, “more carbon monoxide, in preference to carbon dioxide, is emitted.”
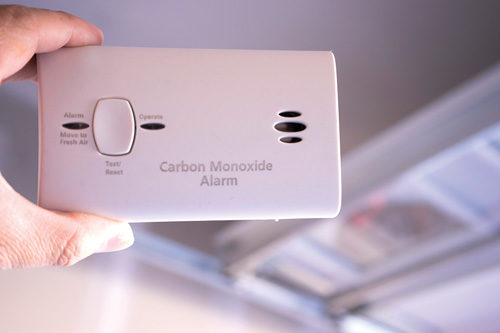
Carbon monoxide can come from vehicle exhaust, fuel-burning furnaces, small gasoline-powered engines, portable gasoline-powered generators, forklifts, propane-powered heaters and more. Because of this, never operate these devices in small, enclosed or unventilated places such as garages or tented-off areas, or inside homes.
Signs of danger
It’s important to know the warning signs of CO poisoning. MDCH recommends paying attention to flu-like symptoms, including headache, dizziness, confusion, fatigue and feeling extremely nauseated – especially if more than one worker is experiencing these signs. To help protect workers, MDCH offers these tips:
- Find out from your employer whether your workplace is in compliance with OSHA’s CO permissible exposure limit.
- Carefully follow the instructions and warning labels on all fuel-powered tools and generators.
- Stay cognizant of ventilation issues, especially when working indoors.
- If you believe a worker may be experiencing CO-poisoning symptoms, move him or her outside immediately, and alert your manager.
- Never ignore CO poisoning symptoms. Get to an emergency room or call 911 if you or your co-workers feel sick. “Carbon monoxide poisoning can be determined by a quick blood test done soon after exposure,” MDCH states, adding that your chances of recovery are better if you’re treated quickly.
Post a comment to this article
Safety+Health welcomes comments that promote respectful dialogue. Please stay on topic. Comments that contain personal attacks, profanity or abusive language – or those aggressively promoting products or services – will be removed. We reserve the right to determine which comments violate our comment policy. (Anonymous comments are welcome; merely skip the “name” field in the comment box. An email address is required but will not be included with your comment.)

