Amid COVID-19, NYCOSH releases workplace ventilation, filtration recommendations
New York — Ventilation and air filtration recommendations are part of a new workplace policy guide on reducing COVID-19 transmission, published by the New York Committee for Occupational Safety and Health, a worker advocacy group.
Released in December and developed in partnership with the Last Mile – a volunteer network focused on getting personal protective equipment to frontline health care workers – the MAD+ Policy Guide lays out key best practices on masking, air ventilation and physical distancing, “along with the need for worker voices to be included in safety and health planning.”
With regard to air ventilation, the guide calls for a minimum of six “air changes” an hour in a mechanical ventilation system, if available. An air change refers to the volume of air in a room being fully replaced with outdoor air and/or recirculated air that has already been properly filtered, the guide states.
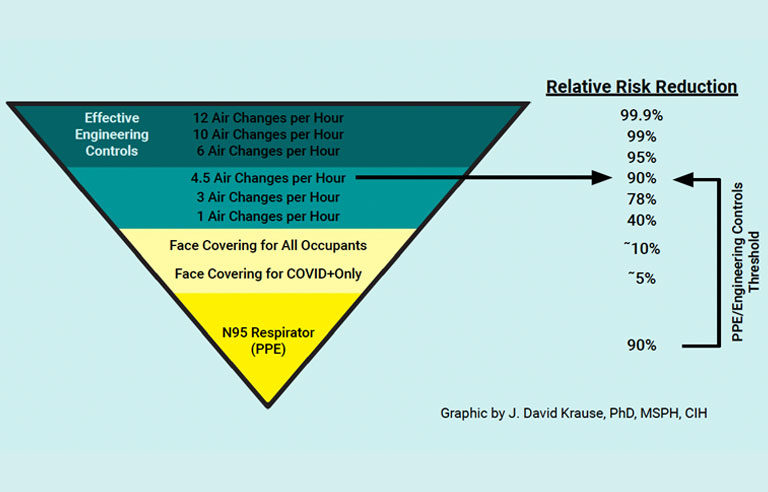
According to a graphic developed by certified industrial hygienist J. David Krause and included in the guide, six air changes or more an hour have a “relative risk reduction” of 95% or greater for COVID-19 transmission. By comparison, one air change an hour has a risk reduction of 40%, while three air changes an hour have a risk reduction around 78%.
In addition, NYCOSH calls for the use of air filters with a minimum efficiency reporting value, or MERV, of 13 or better. According to the guide, filters with a 13-15 MERV capture 50% to 85% of particles that are 0.3 to 1 micron in size. A MERV 16 filter will capture 95% of those particles, and a HEPA filter will capture 99.9% of particles that are 0.3 microns.
Heating, ventilation and air conditioning systems should be used one to two hours before anyone enters the building and two to three hours after everyone has left.
If mechanical ventilation is unavailable, the use of portable filtration devices, the opening of doors and windows (as long as it doesn’t pose a safety risk), and the use of fans to supplement those open windows are recommended.
| Sign up for Safety+Health's free monthly email newsletters and get the news that's important to you. |
Ventilation engineers or industrial hygienists should assess the building’s air flow. NYCOSH suggests the use of carbon dioxide monitors to determine the effectiveness of ventilation. Ideally, indoor CO2 levels should be 600 parts per million or lower. This shows that ventilation is properly removing contaminated air from people exhaling. (Other factors such as whether people are masked, physically distanced and vaccinated will also continue to play a role in whether the room is “COVID safe”).
“We cannot overstate the need to prioritize indoor air quality to support human health,” Kevin Van Den Wymelenberg, advisor to the Last Mile’s COVID Straight Talk Lab and founder of the Institute for Health in the Built Environment, said in a NYCOSH press release. “Enclosed and poorly ventilated spaces, including workplaces at which essential workers are obligated to spend long periods of time for the sake of their livelihoods, continue to present dangers of disease transmission.”
Post a comment to this article
Safety+Health welcomes comments that promote respectful dialogue. Please stay on topic. Comments that contain personal attacks, profanity or abusive language – or those aggressively promoting products or services – will be removed. We reserve the right to determine which comments violate our comment policy. (Anonymous comments are welcome; merely skip the “name” field in the comment box. An email address is required but will not be included with your comment.)

